Caring for the second victims
The care of second victims responds to the following objectives:
- It must be considered that when an adverse event occurs the professional doubts his or her capacity for clinical judgement. It is therefore necessary to adopt measures to ensure the quality of health care, considering that a premise for guaranteeing quality is that professionals feel that they have sufficient capacity to carry out their work in an appropriate environment. A supportive environment, a supportive organisation and an integrated team of professionals are prerequisites for providing optimal care.
- Minimise the negative emotional impact on second victims of unexpected incidents such as adverse events by providing them with the necessary support, which has a positive impact on safety of the following patients to be cared.
- Avoiding non-quality costs, since the individual and social effort involved in training a healthcare professional(s) is cut short when the professional doubts his or her clinical judgement and ability to continue in his or her profession and decides to leave or change position. The feeling of lack of protection reduces the quality of care, causes disaffection among professionals and, in short, makes it difficult, if not impossible provide optimal care. But this approach requires a non-punitive environment were talking about what happened does not have additional negative consequences.
Second Victim Experience and Support Tool (SVEST)
The Second Victim Experience and Support Tool (SVEST) was been created to better understand the needs of the second victims and to assist the implementation of support resources by the institutions.1 It was created and validated in the United States but currently it is also available in other languages.
Using this tool, Burlison et al1 found that the majority of the healthcare workers surveyed would prefer to have a “respected peer to discuss the details of what happened” when asked about the desirability of 7 support options.
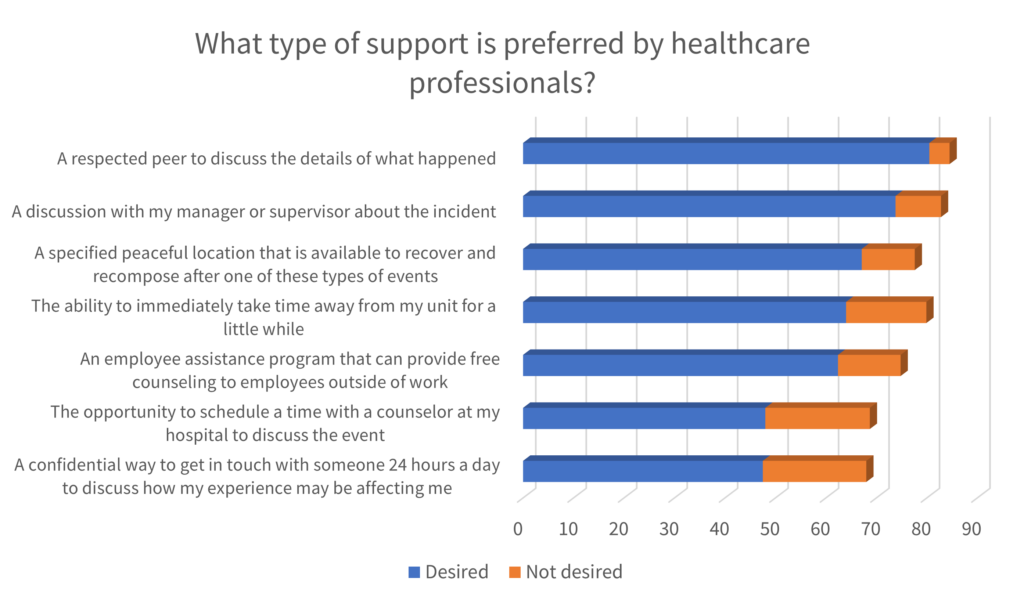
Accordingly, the peer support is the basis of several interventions directed to the second victims.
Peer Support
Peer Support is “emotional first aid” for healthcare providers who are involved in unanticipated adverse patient events, medical errors, or other stressful situations encountered through patient care. Providers involved in such events are often referred to as Second Victims, as they suffer significant emotional, physical, cognitive, and behavioural sequelae in the aftermath of such events. Peer Support is an effective tool in helping staff successfully manage difficult situations, increase resiliency, and decrease burnout.
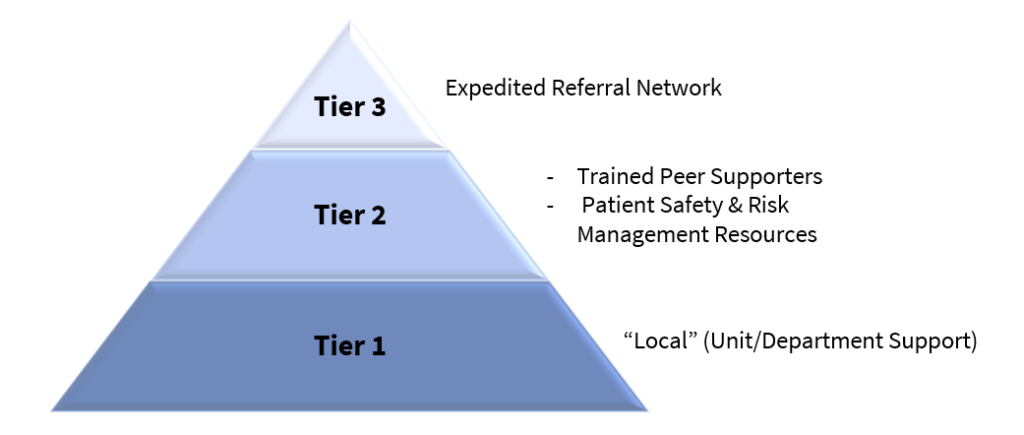
The three-stage intervention model suggested by Susan Scott2 is the most widespread framework to guide the support of second victims. It is based on peer support, first from the unit itself (basic emotional first aid) and at a second level by trained peers. The third level is based on more specialised support.
In most cases, the tier 1 will provide sufficient support to the victims; it is composed by peers and unit leaders that should have received some basic awareness training to the second victim’s needs. When necessary, the second victims can be referred for Tier 2, where specially trained peers can provide guidance and support. When the needs of the second victims exceeds the expertise of the peer supporters, they can be referred for Tier 3, composed by professional counsellors.
In the ERNST Course, different programs to support the second victims are detailed: https://course.cost-ernst.eu/
Improving healthcare workers’ resilience
To protect healthcare workers from becoming second victims it is crucial to increase their resilience, that is the ability of individuals to withstand the stressful situation. 3
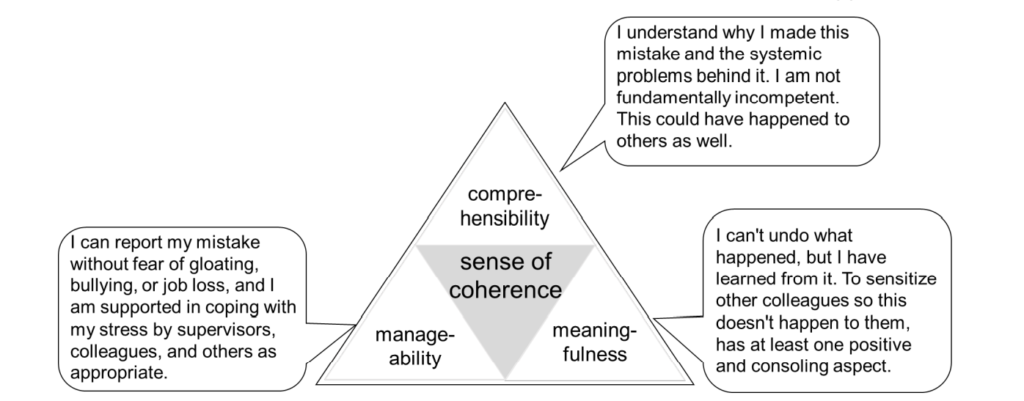
The sociologist Antonovsky described the sense of coherence, which is central to successfully coping with challenges, as a prerequisite for resilience.
The sense of coherence is composed of three domains. When confronted with a stressor, the person with a strong sense of coherence will:
- wish to, be motivated to, cope – meaningfulness.
- believe that the challenge is understood – comprehensibility.
- believe that resources to cope are available – manageability.
In the context of a healthcare environment where a worker was involved in an incident, the sense of coherence theory could be exemplified by the following statements. They illustrate the attitudes of resilient workers:
In terms of organisational support, the following measures should be considered3:
| aspect of SoC | organisational support | measures to achieve this goal |
|---|---|---|
| comprehensibility | guaranteed systematic follow-up of the event with objective complete clarification of the facts of the case | qualification of clinical risk managers to facilitate root-cause-analysis, including the appropriate provision of resourcesinitiation of root-cause-analysis for every second victim problem as part of the risk management strategy |
| manageability | Allow coming to rest enable reporting of the case and complaints in blame-free atmosphere support in coping with the situation as needed | offer interruption of clinical activityestablishes a Just Culture to avoid gossip, bullying, or exclusion. sensitization of staff regarding the rapid recognition of possible second victim problems establishment of appropriate structures for the confidential support of a second victim by experts, if necessary |
| meaningfulness | recognition of the knowledge gained from the error and visibility of the systematic measures derived from it | involvement in the analysis of this case and feedback to prevent future incidents and feedback on derived new preventive measures. establishment of a safety culture that deals constructively and explicitly with mistakes to learn from them |
The COVID-19 pandemic represented a major challenge for everyone. In particular, healthcare workers were exposed to high levels of work, physical exhaustion, emotional stress, and so on. Has become visible the need of caring for those who care.
A set of recommendations were designed, based on Scott’s model and SoC theory. 3 They aim to support the healthcare workers, increasing their resilience and helping to minimize the risk of overwhelming the healthcare system.
Please consult Recommendations: Maintaining capacity in the healthcare system during the COVID‐19 pandemic by reinforcing clinicians’ resilience and supporting second victims
- Burlison, J.D., Scott, S.D., Browne, E.K., Thompson, S.G., & Hoffman JM. The second victim experience and support tool (SVEST): Validation of an organizational resource for assessing second victim effects and the quality of support resources. J Patient Saf. 2017;13(2):93–102.
- SCOTT, Susan D. et al. – Caring for our own: Deploying a systemwide second victim rapid response team. Joint Commission Journal on Quality and Patient Safety. . ISSN 15537250. 36:5 (2010) 233–240. doi: 10.1016/S1553-7250(10)36038-7.
- Strametz R, Raspe M, Ettl B, Huf W, Pitz A. Recommendations: Maintaining capacity in the healthcare system during the COVID‐19 pandemic by reinforcing clinicians’ resilience and supporting second victims. German Coalition for Patient Safety, Austrian Network for Patient Safety; 2020.
0 Comments