Second victims’ symptoms and needs
Busch et al1 conducted a systematic review and meta-analysis to quantify the negative impacts of adverse events on the providers involved. The most prevalent symptoms found were:

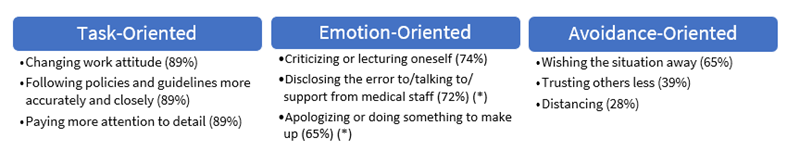
In another study, the same authors also have identified the coping strategies that are applied by the second victims.2 They divided the strategies found into task-oriented, emotion-oriented and avoidance-oriented; the former includes the most frequent strategies found, and the later includes the least-frequently used strategies. Some examples are presented below:
Stages of recovery
In a qualitative exploratory study Scott et al 3 identified the stages of the history of recovery of a second victim. A second victim could pass by the first three stages simultaneously:
| Stage 1: Chaos and intrusive response | |
| Realization about what had occurred Frequently distracted in self-reflection while trying to manage a patient in crisis | How did that happen? Why did that happen? |
| Stage 2: Intrusive reflections | |
| Re-evaluate scenario Feelings of internal inadequacy and periods of self-isolation | What did I miss? Could this have been prevented? |
| Stage 3: Restoring personal integrity | |
| Seeking support of a trusty individual (colleague, family, etc) Managing gossipFear is prevalent | What will others think? Will I ever be trusted again? How much trouble am I in? How come I can’t concentrate? |
| Stage 4: Enduring the inquisition | |
| Realization of level of seriousness Respond to multiple ‘‘why’s’’ about the event Understanding event disclosure to patient/family Physical and psychosocial symptoms | How do I document? Who can I talk to? What happens next? Will I lose my job/license? How much trouble am I in? |
| Stage 5: Obtaining emotional first aid | |
| Seek personal/professional support Getting/receiving help/support Litigation concerns emerge | Why did I respond in this manner? What is wrong with me? Do I need help? Where can I turn for help? |
| Stage 6: Moving on (one of three trajectories chosen) | |
| Dropping out: Transfer to a different unit, considering quitting, feelings of inadequacy | Is this the profession I should be in? Can I handle this kind of work? |
| Surviving: Coping, but still have intrusive thoughts Persistent sadness, trying to learn from event | How could I have prevented this from happening? Why do I still feel so badly/guilty? |
| Thriving Maintain life/work balance Gain insight/perspective Does not base practice/work on one event Advocates for patient safety initiatives | What can I do to improve our patient safety? What can I learn from this? What can I do to make it better? |
Three potential results were described – dropping out, surviving, and thriving -, representing different experiences and career outcomes to the healthcare workers.
In another study4, second victim distress has been associated with absenteeism and turnover intentions. It was found that the organizational support may result in a decrease of second victim’s distress, mediating the relationships between distress-absenteeism and distress-turnover intentions. Thus, the healthcare organizations could have an important role in the outcomes of a second victim experience and should take care of the caregiver.
A second victim need:
- Talk about what happened. Understand why it happened.
- Know what to say and who to talk to.
- Not feel rejected by colleagues, and bosses.
- Emotional rest, cannot continue his/her work that same day.
- Feeling useful helps the mistake never happens again.
- Legal advice.
- Information about the incident investigation.
A second victim DO NOT need:
- To face a blaming attitude and rejection by colleagues and bosses.
- To be a target of rumors.
- Advices to not to talk about the incident and to not to notify.
- To feel that the emotional needs are ignored.
- To feel isolated.
- To be subject of repeated interrogations.
- Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Psychological and Psychosomatic Symptoms of Second Victims of Adverse Events: A Systematic Review and Meta-Analysis. J Patient Saf. 2020;16(2):E61–74.
- Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Dealing With Adverse Events : A Meta-analysis on Second Victims ’ Coping Strategies. J Patient Saf. 2020;16(2):51–60.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Heal Care. 2009;18:325–30.
- Burlison JD, Quillivan RR, Scott SD, Johnson S, Hoffman JM. The Effects of the Second Victim Phenomenon on Work-Related Outcomes: Connecting Self-reported Caregiver Distress to Turnover Intentions and Absenteeism. J Patient Saf. 2021;17(3):195–9.
0 Comments